Cervical degenerative conditions
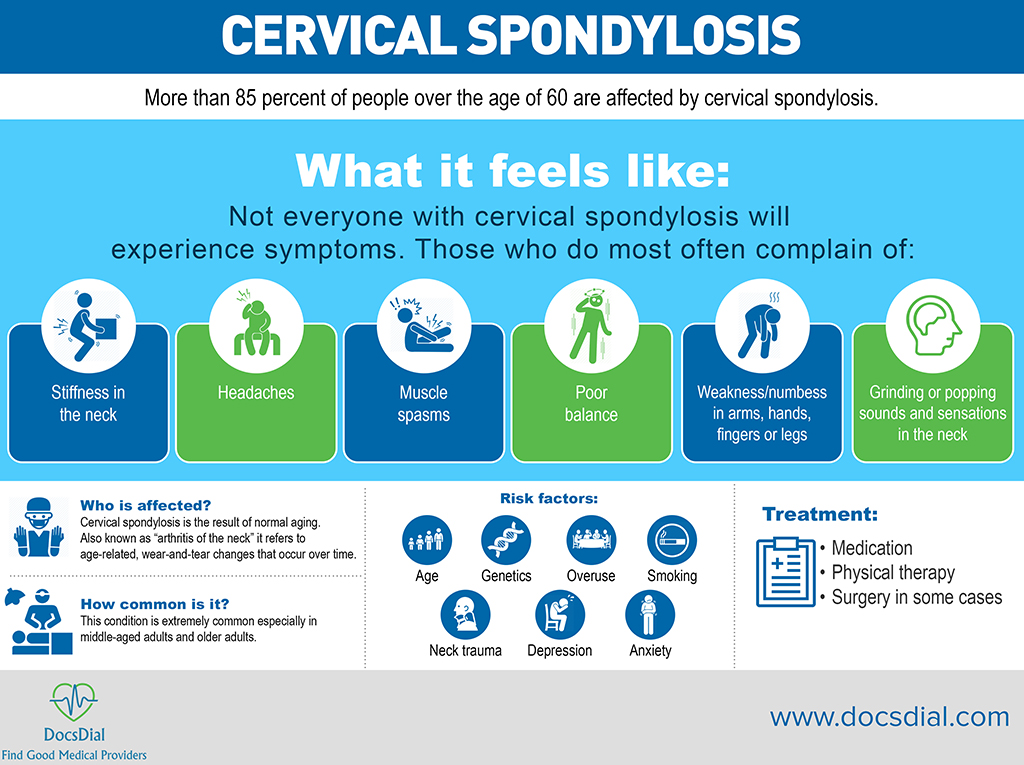
Cervical spondylosis
More than 85 percent of people over the age of 60 are affected by cervical spondylosis.
 What it feels like:
Not everyone with cervical spondylosis will experience symptoms. Those who do most often complain of:
What it feels like:
Not everyone with cervical spondylosis will experience symptoms. Those who do most often complain of:
- Stiffness in the neck
- Headaches
- Muscle spasms
- Poor balance
- Weakness/numbess in arms, hands, fingers or legs
- Grinding or popping sounds and sensations in the neck
- Age
- Genetics
- Overuse
- Smoking
- Neck trauma
- Depression
- Anxiety
- Medication
- Physical therapy
- Surgery in some cases
Neck pain can be caused by many things—but is most often related to getting older. Cervical spondylosis, commonly called arthritis of the neck, is the medical term for these age-related, wear-and-tear changes that occur over time. Cervical spondylosis is extremely common. More than 85 percent of people over the age of 60 are affected. The condition most often causes pain and stiffness in the neck—although many people with cervical spondylosis experience no noticeable symptoms. In most cases, cervical spondylosis responds well to conservative treatment that includes medication and physical therapy. For more information click here: http://orthoinfo.aaos.org/topic.cfm?topic=A00369 or here:http://www.depuysynthes.com/patients/aabp/resources/np
Cervical Radiculopathy
This condition is occurs when a neck nerve is compressed or irritated, resulting in pain.
 What it feels like:
Symptoms of cervical radiculopathy include:
What it feels like:
Symptoms of cervical radiculopathy include:
- Pain the radiates into the shoulder
- Muscle weakness/numbness in arms and hands
- Loss of sensation
- Tingling sensation in the hands and/or fingers
- Sharp or burning pain in the neck and arms
- Age
- Injury
- Genetics
- Medication
- Physical therapy
- Collar
- Steroid injections
- Surgery in some cases
Cervical radiculopathy, commonly called a "pinched nerve" occurs when a nerve in the neck is compressed or irritated where it branches away from the spinal cord. This may cause pain that radiates into the shoulder, as well as muscle weakness and numbness that travels down the arm and into the hand. Cervical radiculopathy is often caused by "wear and tear" changes that occur in the spine as we age, such as arthritis. In younger people, it is most often caused by a sudden injury that results in a herniated disk.I n most cases, cervical radiculopathy responds well to conservative treatment that includes medication and physical therapy. or more information, click here: http://orthoinfo.aaos.org/topic.cfm?topic=A00332 or here:http://www.depuysynthes.com/patients/ aabp/resources/articles_learn/id_51
Cervical stenosis/ myelopathy
Myelopathy is caused by pressure on the spinal cord or nerve root often as a result of spinal stenosis, the narrowing of the spinal canal.
 What it feels like:
Symptoms of myelopathy include:
What it feels like:
Symptoms of myelopathy include:
- Poor balance
- Difficulty walking
- Difficulty using hands and fingers
- Incontinence
- Permanent nerve or spinal cord damage
- Pain weakness, or sensory changes in the back, shoulder, arm or hand
- Spinal stenosis
- Spinal injury
- Spinal infections
- Autoimmune disorders
- Congenital disorders
- Oncological disorders
- Neurological discorders
- Decompression surgery
Most cervical problems are due to degenerative changes that occur in the discs and joints of the neck. Degenerative changes that affect the structures of the spine can cause the spinal canal to become too narrow, a condition called spinal stenosis. This may lead to pressure on the spinal cord. Bone spurs that stick into the spinal canal take up space, making the spinal canal smaller. They can press against the spinal cord or nerve roots. Pressure on the spinal cord from spinal stenosis can cause symptoms of myelopathy. Myelopathy may impair normal walking, hand and finger use, and bowel and bladder function. Doctors take these symptoms very seriously because severe myelopathy that is not treated may lead to permanent nerve or spinal cord damage. Pressure on nearby nerve roots can cause radiculopathy and may produce pain, weakness, or sensory changes in the area supplied by nerves that go from the cervical spine to the shoulder, arm, or hand. For more information click here: http://www.depuysynthes.com/patients/ aabp/resources/articles_learn/id_52
Lumbar degenerative conditions
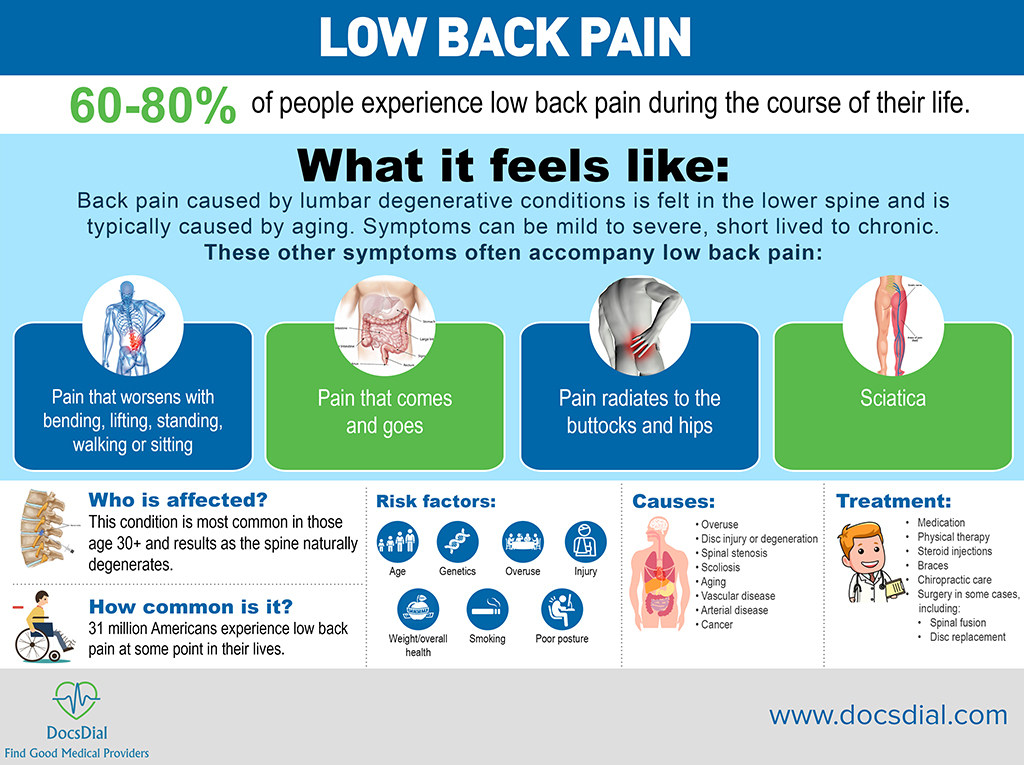
Low Back Pain
60-80% of people experience low back pain during the course of their life.
 What it feels like:
Back pain caused by lumbar degenerative conditions is felt in the lower spine and is typically caused by aging. Symptoms can be mild to severe, short lived to chronic.
These other symptoms often accompany low back pain:
What it feels like:
Back pain caused by lumbar degenerative conditions is felt in the lower spine and is typically caused by aging. Symptoms can be mild to severe, short lived to chronic.
These other symptoms often accompany low back pain:
- Pain that worsens with bending, lifting, standing, walking or sitting
- Pain that comes and goes
- Pain radiates to the buttocks and hips
- Sciatica
- Age
- Genetics
- Overuse
- Injury
- Weight/overall health
- Smoking
- Poor posture
- Overuse
- Disc injury or degeneration
- Spinal stenosis
- Scoliosis
- Aging
- Vascular disease
- Arterial disease
- Cancer
- Medication
- Physical therapy
- Steroid injections
- Braces
- Chiropractic care
- Surgery in some cases, including:
- Spinal fusion
- Disc replacement
Almost everyone will experience low back pain at some point in their lives. This pain can vary from mild to severe. It can be short-lived or long-lasting. However it happens, low back pain can make many everyday activities difficult to do. For more information click here: http://orthoinfo.aaos.org/topic.cfm?topic=A00311 or here: http://www.depuysynthes.com/patients/aabp/resources/lp
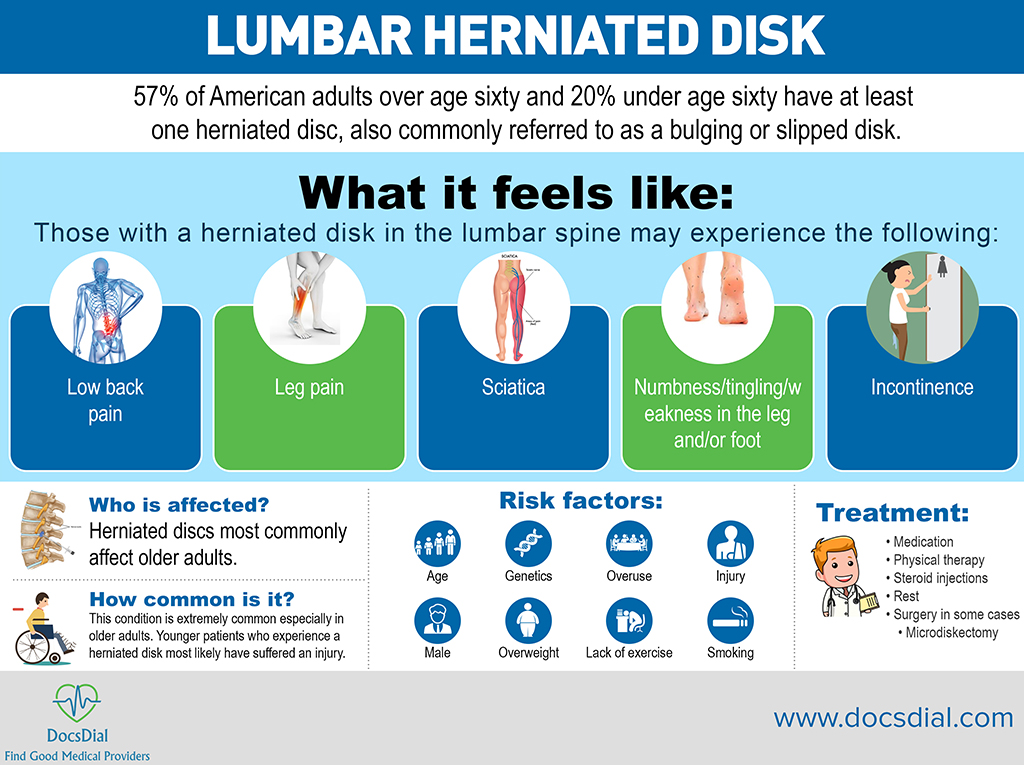
Lumbar disc herniation
57% of American adults over age sixty and 20% under age sixty have at least one herniated disc, also commonly referred to as a bulging or slipped disk.
 What it feels like:
Those with a herniated disk in the lumbar spine may experience the following:
What it feels like:
Those with a herniated disk in the lumbar spine may experience the following:
- Low back pain
- Leg pain
- Sciatica
- Numbness/tingling/weakness in the leg and/or foot
- Incontinence
- Age
- Genetics
- Overuse
- Injury
- Male
- Overweight
- Lack of exercise
- Smoking
- Occupation that requires long periods of sitting
- Medication
- Physical therapy
- Steroid injections
- Rest
- Surgery in some cases
-
- Microdiskectomy
-
Sometimes called a slipped or ruptured disk, a herniated disk most often occurs in your lower back. It is one of the most common causes of low back pain, as well as leg pain (sciatica). Between 60% and 80% of people will experience low back pain at some point in their lives. A high percentage of people will have low back and leg pain caused by a herniated disk. Although a herniated disk can sometimes be very painful, most people feel much better with just a few weeks or months of nonsurgical treatment. For more information click here: http://orthoinfo.aaos.org/topic.cfm?topic=A00534 or here: http://www.depuysynthes.com/patients/ aabp/resources/ddd
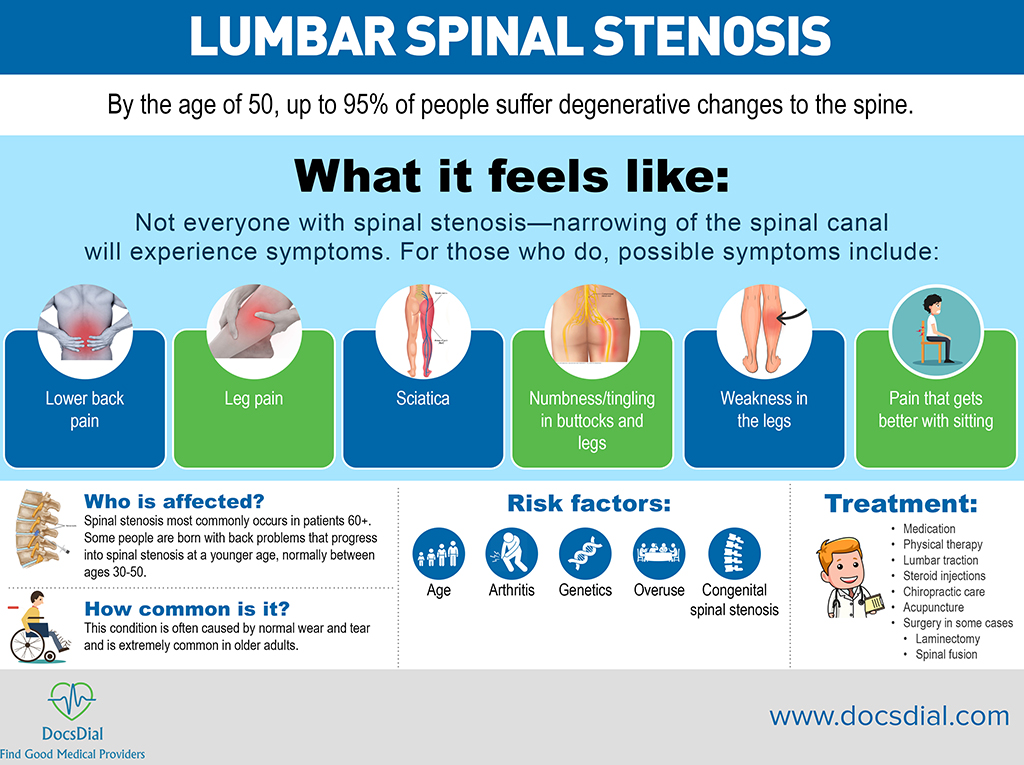
Lumbar spinal stenosis
By the age of 50, up to 95% of people suffer degenerative changes to the spine.
 What it feels like:
Not everyone with spinal stenosis—narrowing of the spinal canal—will experience symptoms. For those who do, possible symptoms include:
What it feels like:
Not everyone with spinal stenosis—narrowing of the spinal canal—will experience symptoms. For those who do, possible symptoms include:
- Lower back pain
- Leg pain
- Sciatica
- Numbness/tingling in buttocks and legs
- Weakness in the legs
- Pain that gets better with sitting
- Age
- Arthritis
- Genetics
- Overuse
- Congenital spinal stenosis
- Medication
- Physical therapy
- Lumbar traction
- Steroid injections
- Chiropractic care
- Acupuncture
- Surgery in some cases
-
- Laminectomy
- Spinal fusion
-
A common cause of low back and leg pain is lumbar spinal stenosis. As we age, our spines change. These normal wear-and-tear effects of aging can lead to narrowing of the spinal canal. This condition is called spinal stenosis. Degenerative changes of the spine are seen in up to 95% of people by the age of 50. Spinal stenosis most often occurs in adults over 60 years old. Pressure on the nerve roots is equally common in men and women. A small number of people are born with back problems that develop into lumbar spinal stenosis. This is known as congenital spinal stenosis. It occurs most often in men. People usually first notice symptoms between the ages of 30 and 50. For more information click here: http://orthoinfo.aaos.org/topic.cfm?topic=A00329 or here: http://www.depuysynthes.com/patients/ aabp/resources/articles_learn/id_23
Peripheral nerve conditions
Carpal tunnel syndrome is a peripheral nerve condition that occurs when the median nerve is squeezed.
 What it feels like:
Those who suffer from carpal tunnel syndrome may experience the following:
What it feels like:
Those who suffer from carpal tunnel syndrome may experience the following:
- Pain/numbness/weakness/tingling in hand, shoulder or arm
- Shock-like sensations that radiate to the fingers
- Clumsiness while using hands/Dropping items
- Genetics
- Overuse
- Pregnancy
- Arthritis
- Diabetes
- Other health issues
- Gender
- Age
- Medication
- Rest
- Physical therapy
- Steroid injections
- Surgery in some cases
-
- Carpal tunnel release (open)
- Carpal tunnel release (endoscopic)
-
Peripheral nerve conditions can cause pain, numbness, and tingling in the hand and arm. The condition occurs when one of the major nerves to the hand is squeezed or compressed as it travels through the elbow or wrist. The condition can worsen over time, so treatment is important and continued pressure on the nerves can cause permanent damage. For more information on carpal tunnel syndrome: http://orthoinfo.aaos.org/topic.cfm?topic=A00005 For more information on cubital tunnel syndrome: http://orthoinfo.aaos.org/topic.cfm?topic=A00069
Arthritis
Arthritis is the leading cause of disability amongst U.S. adults.
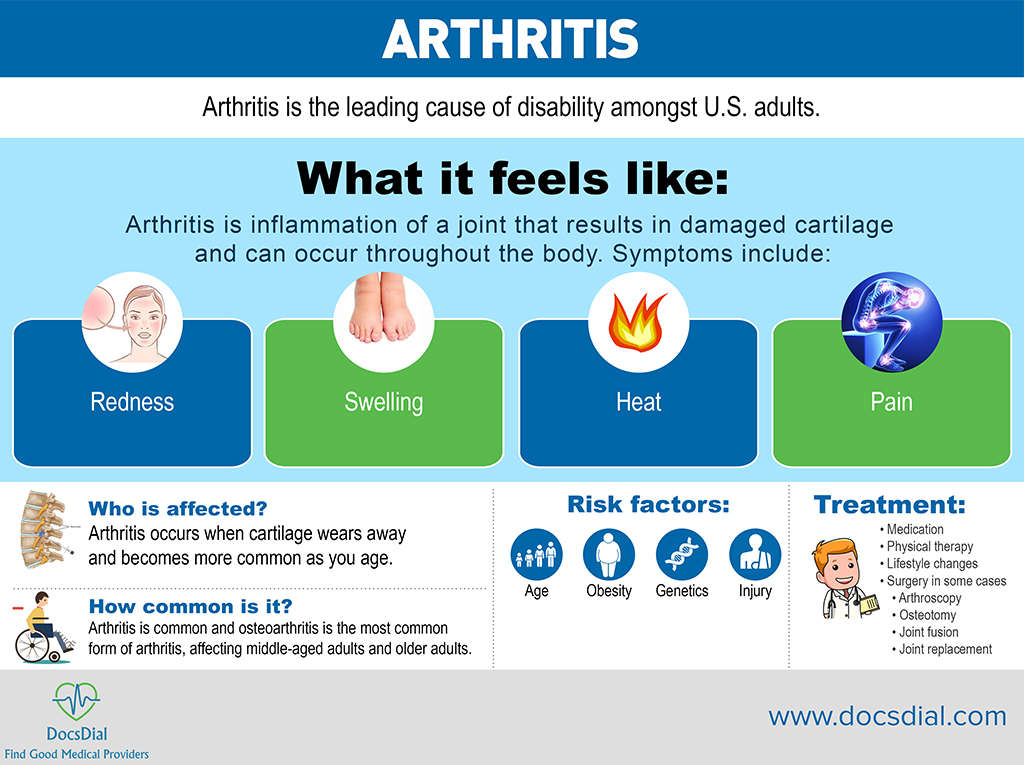 What it feels like:
Arthritis is inflammation of a joint that results in damaged cartilage and can occur throughout the body. Symptoms include:
What it feels like:
Arthritis is inflammation of a joint that results in damaged cartilage and can occur throughout the body. Symptoms include:
- Redness
- Swelling
- Heat
- Pain
- Age
- Obesity
- Genetics
- Injury
- Medication
- Physical therapy
- Lifestyle changes
- Surgery in some cases
-
- Arthroscopy
- Osteotomy
- Joint fusion
- Joint replacement
-
Arthritis is a general term covering more than 100 different conditions. The term arthritis literally means inflammation of a joint, but is generally used to describe any condition in which there is damage to the cartilage. Inflammation is the body's natural response to injury. The warning signs that inflammation presents are redness, swelling, heat and pain. The cartilage is a padding that absorbs stress. The proportion of cartilage damage and synovial inflammation varies with the type and stage of arthritis. Usually the pain early on is due to inflammation. In the later stages, when the cartilage is worn away, most of the pain comes from the mechanical friction of raw bones rubbing on each other. For more information, click the following links from the Academy of Orthopedic Surgery website: Arthritis: http://www.orthoinfo.org/topic.cfm?topic=A00227 Knee arthritis: http://www.orthoinfo.org/topic.cfm?topic=A00212 Hip arthritis: http://www.orthoinfo.org/topic.cfm?topic=A00213
Knee/Hip replacement
Knee and hip replacement procedures are the third and fourth most common surgeries performed in the United States.
 What it feels like:
A knee or hip replacement is needed when the joint has been damaged by arthritis, fracture or other injury:
What it feels like:
A knee or hip replacement is needed when the joint has been damaged by arthritis, fracture or other injury:
- Pain
- Poor range of motion
- Difficulty doing daily activities
- Age
- Genetics
- Arthritis
- Injury
- Surgery
-
- Total hip replacement
- Total knee replacement
- Partial hip replacement
- Partial knee replacement
- Conformis joint replacements
-
Dr. Abbi is proficient at hip and knee replacement having performed hundreds of these procedures throughout his career. Hip joint and knee joint replacements are helping people of all ages live pain- free, active lives. Joints are formed by the ends of two or more bones connected by tissue called cartilage. Healthy cartilage serves as a protective cushion, allowing smooth and low-friction movement of the joint. If the cartilage becomes damaged by disease or injury, the tissues around the joint become inflamed, causing pain. With time, the cartilage wears away, allowing the rough edges of bone to rub against each other, causing more pain. When only some of the joint is damaged, a surgeon may be able to repair or replace just the damaged parts. When the entire joint is damaged, a total joint replacement is done. To replace a total hip or knee joint, a surgeon removes the diseased or damaged parts and inserts artificial parts, called prostheses or implants. For more information regarding Hip replacement, click: http://orthoinfo.aaos.org/topic.cfm?topic=A00377 or http://www.depuysynthes.com/patients/hip/ patient-treatment-center/hip-replacement For more information regarding Knee replacement, click: http://orthoinfo.aaos.org/topic.cfm?topic=A00389 or http://www.depuysynthes.com/patients/knee/ patient-treatment-center/knee-replacement
Fracture Care 101
What is a fracture? A fracture is a medical term for a broken bone. Fractures are common and can happen to people of any age. There are several different types of fractures and some medical conditions that can make some patients more susceptible to fractures. Types of fractures? There are many different kinds of fracture. Here we will highlight five basic types.
- Stable fracture: With a stable fracture, the ends of the broken bone are barely out of place and do not need any realignment.
- Open, compound fracture: An open, compound fracture occurs when the force of the break causes an open wound, or the bone goes through the skin where the fracture happened.
- Transverse fracture: A transverse fracture occurs in a horizontal line across the bone.
- Oblique fracture: An oblique fracture causes the bone to break on an angle.
- Comminuted fracture: When this type of fracture occurs, the bone shatters into three or more pieces.
 Symptoms of a fracture
Even though there are many different ways that a fracture can occur, there are primary symptoms that are present whenever a bone breaks. These symptoms can include pain, swelling, tenderness, bruising, numbness or tingling, difficulty moving the injured body part, and deformity
Fracture risk factors
Different things can cause a person to be at a higher risk of suffering a bone fracture. Some of the risk factors include:
Symptoms of a fracture
Even though there are many different ways that a fracture can occur, there are primary symptoms that are present whenever a bone breaks. These symptoms can include pain, swelling, tenderness, bruising, numbness or tingling, difficulty moving the injured body part, and deformity
Fracture risk factors
Different things can cause a person to be at a higher risk of suffering a bone fracture. Some of the risk factors include:
- Age: Bone loss and structural damage with aging can lead to fragile bones. Statistics have shown that fragility fractures exceed 2 million each year in the United States.
- Gender: According to the National Osteoporosis Foundation, up to one-half of the women that are over 50 will experience a bone fracture in their lifetime. This is primarily the result of postmenopausal bone loss.
- Diseases: These include rheumatoid arthritis, osteoporosis, Crohn’s disease, ulcerative colitis and celiac disease, primary hyperparathyroidism, chronic kidney disease, chronic liver disease, COPD, diabetes, untreated hyperthyroidism, and certain neurological disorders.
- Medications: These medications are included because they can cause bone loss, falls, and fractures. They include synthetic glucocorticoids (prednisone, dexamethasone), cancer drugs, proton pump inhibitors for heartburn, contraceptive Depo-Provera, anti-seizure drugs, some antidepressants, sleep and antipsychotic medications, medications for hypertension, diuretics, prostate drugs, and others.
Osteoporosis
Osteoporosis is responsible for more than 2 million fractures every year.
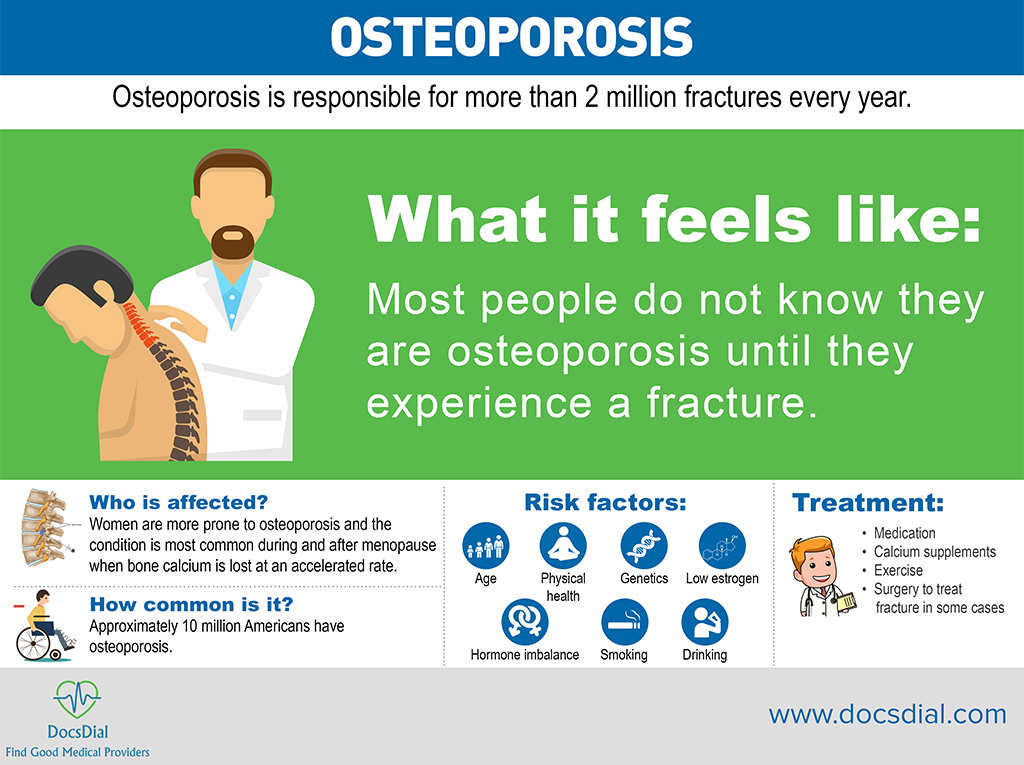 What it feels like:
Most people do not know they are osteoporosis until they experience a fracture.
Who is affected?
Women are more prone to osteoporosis and the condition is most common during and after menopause when bone calcium is lost at an accelerated rate.
How common is it?
Approximately 10 million Americans have osteoporosis.
Risk factors:
What it feels like:
Most people do not know they are osteoporosis until they experience a fracture.
Who is affected?
Women are more prone to osteoporosis and the condition is most common during and after menopause when bone calcium is lost at an accelerated rate.
How common is it?
Approximately 10 million Americans have osteoporosis.
Risk factors:
- Age
- Physical health
- Genetics
- Low estrogen
- Hormone imbalance
- Smoking
- Drinking
- Medication
- Calcium supplements
- Exercise
- Surgery to treat fracture in some cases
Osteoporosis prevention is key especially the elderly population. For more information, click here: http://orthoinfo.aaos.org/topic.cfm?topic=A00315
Lumbar spondylolisthesis
This condition occurs when a vertebrae slips forward and out of place.
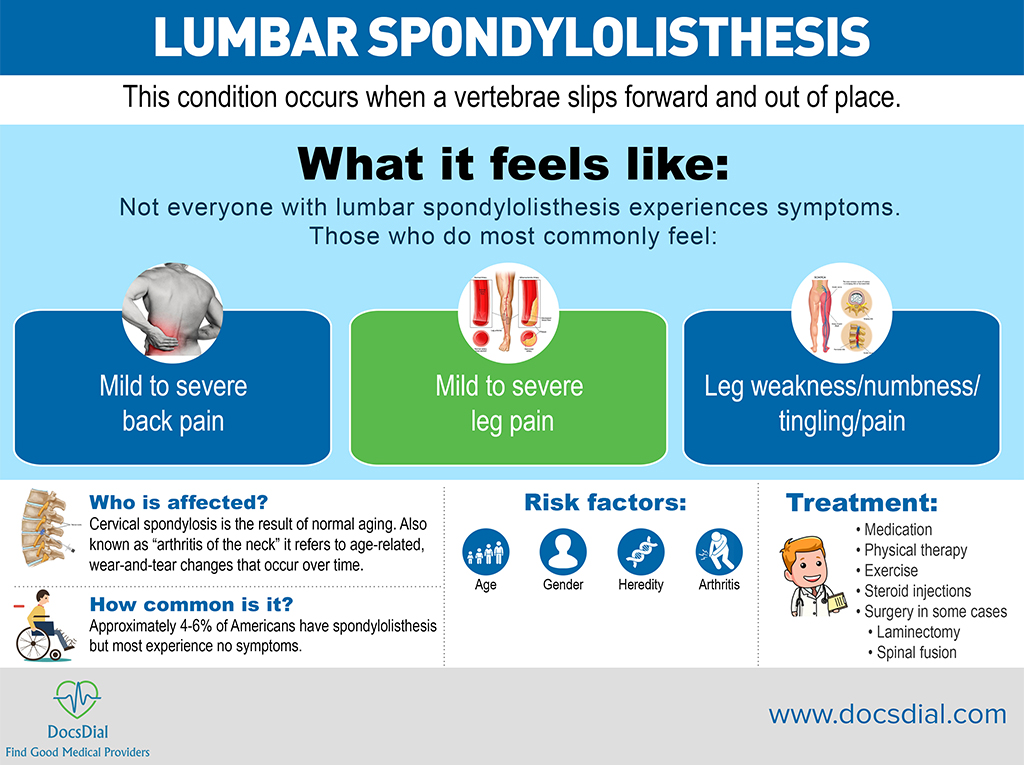 What it feels like:
Not everyone with lumbar spondylolisthesis experiences symptoms. Those who do most commonly feel:
What it feels like:
Not everyone with lumbar spondylolisthesis experiences symptoms. Those who do most commonly feel:
- Mild to severe back pain
- Mild to severe leg pain
- Leg weakness/numbness/tingling/pain
- Age
- Gender
- Heredity
- Arthritis
- Medication
- Physical therapy
- Exercise
- Steroid injections
- Surgery in some cases
-
- Laminectomy
- Spinal fusion
-
In spondylolisthesis, one of the bones in your spine — called a vertebra — slips forward and out of place. This may occur anywhere along the spine, but is most common in the lower back (lumbar spine). In some people, this causes no symptoms at all. Others may have back and leg pain that ranges from mild to severe. For more information click here: For more information click here: http://orthoinfo.aaos.org/topic.cfm?topic=A00588
