Anterior Cervical Discectomy and Fusion

San Francisco neck pain sufferers -- Eliminate neck pain with Anterior Cervical Discectomy Fusion surgery!
83% of patients find relief from neck pain with ACDF surgery.
100% of patients receive arm pain relief after surgery.
Why do San Francisco patients undergo ACDF? As we age, the cervical disks in our spine begin to collapse and bulge, which causes a loss of space between cervical vertebrae. Cervical disk degeneration happens to everyone, usually by age 60, but some experience worse degeneration than others. Scientists aren’t sure why it happens, but for those with advanced cervical disk degeneration, surgery may be needed.
In some cases, disks are damaged due to injury instead of degeneration.
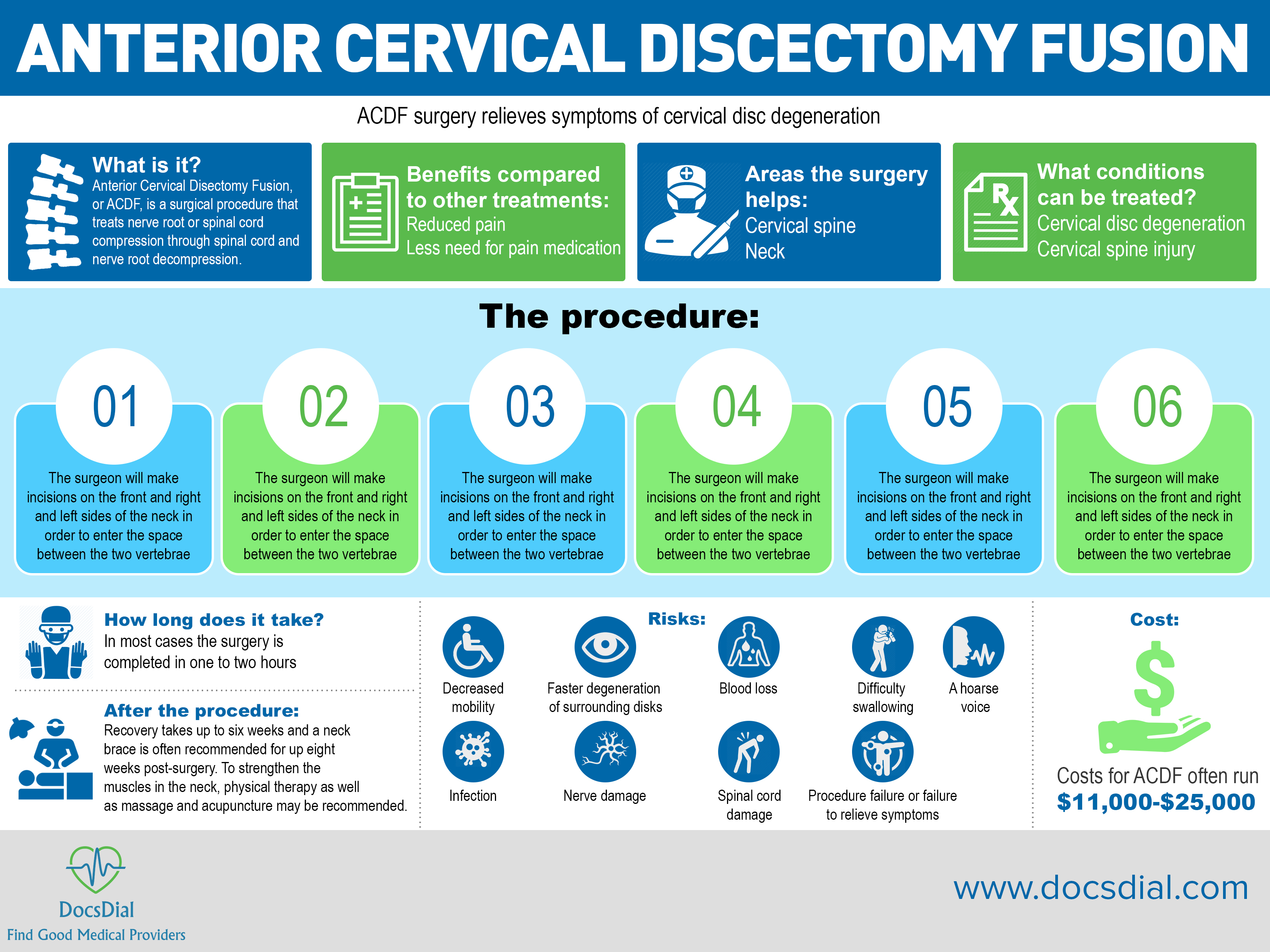
What is it?
The cervical spine is made up of seven bones or vertebrae stacked one on top of another forming the neck. In between the vertebrae are cushions called disks. These act as shock absorbers so when they deteriorate with age, the neck can become painful and hard to move. Loss of mobility with cervical disk degeneration is common.
Because the upper part of the spinal cord passes through the cervical spine, the vertebrae or cervical disk can press on it when the opening becomes too narrow. Sometimes, the body reacts to a disrupted disk by forming bone spurs, which can also put pressure on the spinal nerves, causing neck pain. Pushing against the spinal nerves leads to pain, numbness and sometimes weakness in the neck and extremities. When nonsurgical treatments do not provide relief, surgery is often recommended.
Anterior Cervical Disectomy Fusion in San Francisco treats nerve root or spinal cord compression through spinal cord and nerve root decompression. The goal is to stabilize the surrounding vertebrae where the disk has deteriorated and eliminate or reduce chronic neck pain in San Francisco patients. In most cases, a nerve root becomes inflamed because the disk has herniated allowing the jelly-like center of the disc to bulge through and put pressure on the nerve root or because the disc has degenerated and the cushion is no longer there to protect it.
Purpose
The goal of ACDF surgery is to eliminate pain caused by a pinched nerve or several pinched nerves in the neck or cervical spine. ACDF surgery is often recommended over other procedures if arm pain caused by a pinched nerve root is a main concern. Only about half of patients will feel reduced neck pain after the procedure.
Benefits
ACDF surgery is done to alleviate severe symptoms associated with cervical disk degeneration, which include: neck stiffness, neck pain, headache, pain that travels into the shoulders and arms, weakness in hands, arms, shoulders and legs and numbness in the arms. Those who experience severe arm pain are often the best candidates for San Francisco ACDF surgery.
Areas the surgery helps:
San Francisco ACDF surgery reduces or eliminates back pain in the cervical spine and neck.
What conditions can be treated?
San Francisco ACDF surgery treats cervical disc degeneration and cervical spine injury.
The procedure:
San Francisco ACDF surgery used to relieve neck pain takes between one and two hours in most cases, form start to finish.
Here’s how a routine procedure goes:
- Dr. Abbi will make incisions on the front and right and left sides of the neck in order to enter the space between the two vertebrae, moving your esophagus and trachea aside
- The damaged disk and bone spurs will be removed, called a diskectomy
- A drill is used to widen the opening the spinal cord runs through to eliminate pressure
- The vertebrae are then fused using a bone graft with bone harvested from yourself or a donor
- If more than one disc has been damaged or if more stabilization is needed, a titanium plate or screws may be used to reinforce the vertebrae
- The incisions are closed with sutures and you are wheeled to recovery
After the Procedure
Recovery is gradual and often takes up to six weeks. One to three days of that recovery will be done in the hospital or clinic where Dr. Abbi performed the surgery. Using an endoscopic micro discectomy instead can reduce recovery to just a couple of days. To maintain proper spinal alignment and prevent injury from too much movement, a neck brace is often recommended for up eight weeks post-surgery. To strengthen the muscles in the neck, physical therapy as well as massage and acupuncture may be recommended.
Alternatives
Before surgical intervention, most patients will try a mix of physical therapy and pain medication to alleviate symptoms associated with degenerative disk disease. In some cases, steroid injections will be given in the spine or traction will be done to reduce symptoms. Other surgical methods include cervical total disk replacement surgery (a newer procedure during which an artificial disc is placed in the space between the vertebrae where the old one was removed). Posterior discectomy and lamino-foraminotomy are also surgical options for treating cervical disc degeneration.
Risks
When several vertebrae are fused together, a decrease in mobility may be experienced. Patients may be able to feel the difference with only one fusion in some activities that require a lot of neck movement. Most, however, do not experience a significant change in movement and many actually report better movement after surgery. When vertebrae are fused together, motion is eliminated in that part of the spine, which can lead to faster degeneration of surrounding disks and require subsequent surgeries. Other risks include blood loss, which could require the need for a blood transfusion, difficulty swallowing, a hoarse voice, infection, nerve damage, spinal cord damage, procedure failure (occurring in 1 in 50 cases) and failure to relieve symptoms.
After surgery it is important to get up and move as soon as possible to avoid complications from extended bed rest including risk of deep vein thrombosis (blood clots in the deep veins) and bed sores.
Dr. Abbi performs ACDF surgery in San Francisco to relive neck pain, arm pain and numbness or weakness in the neck and extremities caused by a pinched nerve.
Payments/cost
Costs for San Francisco ACDF often run $11,000-$25,000. How many discs are treated will affect cost. Insurance will likely cover some or all of the procedure, so check with your provider for an accurate estimate of out of pocket expenses. Don’t forget to factor in aftercare, including physical therapy.
References:
North American Spine Society (February 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, North American Spine Society, retrieved 25 March 2013
"Costs for Spinal Fusion Vary Substantially by Region, Shows New Research." News-Medical.net. September 02, 2015. Accessed May 01, 2018. https://www.news-medical.net/news/20150902/Costs-for-spinal-fusion-vary-substantially-by-region-shows-new-research.aspx.
https://intermountainhealthcare.org/ext/Dcmnt?ncid=520444815
When symptoms of cervical radiculopathy persist or worsen despite nonsurgical treatment, your doctor may recommend surgery. The primary goal of surgery is to relieve your symptoms by decompressing, or relieving pressure on, the compressed nerves in your neck. Other goals of surgery include:
- Improving neck pain
- Maintaining stability of the spine
- Improving alignment of the spine
- Preserving range of motion in the neck
In most cases, surgery for cervical radiculopathy involves removing pieces of bone or soft tissue (such as a herniated disk)—or both. This relieves pressure by creating more space for the nerves to exit the spinal canal.
For more information click:
http://www.orthoinfo.org/topic.cfm?topic=A00540
or here:
http://www.depuysynthes.com/patients/aabp/resources/articles_learn/id_54
Posterior Cervical Surgery
San Francisco neck pain sufferers – get relief with posterior cervical surgery patients
95 to 98% pain relief from symptoms in majority of patients from San Francisco posterior cervical surgery.
80-90 percent of San Francisco arm pain suffered report excellent or great results from this procedure.
Neck or upper spinal surgery with the access point being from the posterior (back) postion. It is often referred to as a cervical foraminotomy.

What is it?
Posterior Cervical surgery is a spine surgery used to treat issues in the cervical (upper) spine. The word “posterior” refers to Dr. Abbi’s access point to the spine coming from the posterior or back location rather then from the anterior or front location. In most cases this surgery is performed through tiny incisions and often offered as a minimally invasive procedure. In some cases, however, it is performed as an open procedure. A drill is used during the procedure to widen the space where a nerve passes through the spine.Purpose
The purpose of this procedure is to remove pressure in the cervical spine that causes neck and/or arm pain in the patient. Accessing the affected nerve root and removing disk bulges or anything else that may be putting pressure on the spine achieve this.Benefits:
This procedure is most commonly performed as a minimally invasive surgery. Like all other minimally invasive procedures, it allows patients a faster surgery, a short hospital stay or no stay at all and a faster recovery. With the smaller incisions, there is also less blood loss and reduced pan during recovery.Areas the procedure helps:
The San Francisco posterior cervical surgery, done on the cervical spine (upper back), relieves pain in the neck, cervical spine and arms.What conditions can be treated?
The San Francisco posterior cervical surgery relieves symptoms associated with radiculopathy, myelopathy, instability caused by degeneration or trauma, infection, tumors and compression.The procedure:
The posterior cervical surgery generally takes up to one hour and fifteen minutes to complete. This does not include pre-op and post-op anesthesia times nor does it include time in recovery.- Before surgery, the patient is anesthetisized and may be given numbing medicine to help with pain.
- Dr. Abbi will make an incision into the skin, through the patient’s back.
- Through the incision, usually tiny ones, the disc will be removed.
- A graft will then be inserted where the disc was.
- The bones above and below the disc will be fused to the graft.
- The incision will then be closed with either sutures or staples.
- The patient will be wheeled to recovery.
Risks:
Every surgery carries risks. Anesthesia complications can include death, stroke, deep vein thrombosis, pulmonary embolism and drug allergy. However, San Francisco posterior cervical surgery carries its own set of risks, as well. Sometimes there can be issues with positioning, bone grafting, wound infection, discitis, cervical traction, dural tear or CSF leak. Many of these complications are possible in all spinal surgeries, while others are more closely linked to posterior cervical procedures.After the procedure:
Patients should expect to be monitored closely in the recovery areas following the procedure and administered pain medication and fluids as needed. In many cases the patient will be released the same day, however, sometimes patients will need to stay in the hospital for 1-2 nights. After being released, some patients may need to wear a neck brace for a specified amount of time. In about 1-2 weeks, patients may return to some normal activities including light work, however, a return to regular activity can take up to six weeks.Cost:
The cost of San Francisco posterior cervical surgery typically runs from $8,500 to $9,000 dollars for the surgery alone, not including anesthesia, operating room facilities or other hospital costs, which are typically billed separately. Insurance affects the out-of-pocket costs for patients.Occasionally cervical disc herniation can be address posteriorly. Cervical foraminotomy is the specific name for the procedure performed from the back to alleviate pressure on nerves which are compressed due to a one sided disc herniation. A small hole is made on one side of thelamina, the bone in the back, and any bone or soft tissue that is compressing the nerve is removed. The bone that is removed surgically is not important for the structural support of the spine so removing this bone does not lead to instability or dysfunction. When symptoms of cervical spondylotic myelopathy (CSM) perist or worsen despite nonsurgical treatment, your doctor may recommend surgery.The goal of surgery is to relieve symptoms by "decompressing," or relieving pressure on, the spinal cord. This involves removing the pieces of bone or soft tissue (such as a herniated disk) that may be taking up space in the spinal canal. This relieves pressure by creating more space for the spinal cord.
Posterior Cervical Laminoplasty
San Francisco spinal stenosis patients find relief from neck pain through posterior cervical laminoplasty.
3 in 4 patients experience significant pain relief after a cervical laminoplasty.
Undergo a San Francisco posterior cervical laminoplasty if you suffer from spinal cord compression at multiple levels, a preserved lordotic curvature, congential cervical stenosis, a large anterior herniated disc(s) and/or bone spur(s).
The posterior approach means that the lamina is reached and decompressed through the back instead of the front.
What is it?
The Posterior Cervical Laminoplasty is a surgical procedure that treats spinal cord compression and other defects in the spine, reducing pain at multiple levels especially the neck. In the cervical spine, this procedure is best at reducing neck pain for San Francisco sufferers, and “posterior” simply means that the spine is accessed through incisions in the back instead of through the front, which is referred to as an anterior approach. A laminoplasty works by removing pressure from the cervical spine (often called spinal stenosis), allowing the spine to heal and then reversing symptoms.Purpose
The main purpose of San Francisco posterior cervical laminoplasty is to reduce pain felt in the neck. This pain often leads to problems including myleopathy, which causes numbness, pain, and weakness in the arms and hands, as well as issues with motor skills and balance. By reversing the compression on the spine, these symptoms tend to resolve, making it easier for patients to perform daily tasks free of pain.Benefits
The biggest benefit to undergoing a San Francisco posterior cervical laminoplasty is pain relief. The surgery targets areas of the spine that are compressed, causing pain and pressure mostly in the neck. A huge benefit of posterior cervical laminoplasty over other surgeries that relieve pain associated with spinal stenosis is maintained stability of the spine. Even when performed at multiple levels, which is typically the case with a posterior approach, the spine is able to remain stable while also preserving motion at multiple levels, reducing stiffness and making it easier for patients to move naturally after surgery. As a result of these benefits, patients can stop relying on pain medication to make it through the day.Areas the Surgery Helps:
San Francisco posterior cervical laminoplasty reduces or eliminates cervical spine pain and neck pain.What conditions can be treated?
San Francisco posterior cervical laminoplasty surgery solves symptoms related to congential cervical stenosis, herniated discs, bone spurs, curvature of the spine, spinal cord compression and myleopathy.The procedure:
In most cases posterior cervical laminoplasty is completed in two to four hours. This often is dependent on how many levels need to be operated on.- The patient is placed under general anesthesia and laid face-down on the table. Surgical pins may be used to limit motion during the procedure.
- The surgeon makes a cut in the back of the neck and the muscles are detached from the lamina.
- The lamina are then cut from the facet joints on one side.
- A cut is made on the reverse side.
- The lamina is removed from the spinal cord, relieving pressure that causes pain.
- A bone graft is used and often a small titanium plate as well to reattach the lamina to the facet bone.
- In some cases a fusion may be completed at the same time as the laminoplasty.
- The patient is closed and wheeled to recovery.
Risks
Every surgery comes with a set of risks. Being healthy and happy prior to surgery is the best way to combat complications. Some people may be susceptible to complications with anesthetia, including death, stroke, blood clots in the deep veins, pulmonary embolism and drug allergy. Other complications are rare but can include: bleeding that can lead to a blood transfusion, blood clots, infection, lung problems, spinal cord and nerve injury, spinal fluid leak, problems with the implant or instruments used to stabilize the spine, nonunion that occurs if a fusion does not heal as planned and dural tear. In some cases patients do not experience total or significant pain relief, and the procedure could lead to the need to have a fusion at a later date to maintain spinal stability.After the procedure:
Most patients can expect to stay in the hospital for 2-3 days after surgery and wear a neck brace for a few weeks. A full recovery including pain relief and relief from other symptoms can take up to 18 months but it happens gradually.Alternatives:
Discuss options for spinal surgery with Dr. Abbi. San Francisco neck pain sufferers will most likely want to target a cervical procedure to reduce pressure in the area. The most common altnerative to this procedure would be an anterior cervical laminoplasty. This procedure offers much the same benefits but is ideal for patients with a slightly different presentation. For example, if only one level needs to be addressed, doctors may use an anterior approach instead, while the posterior approach is ideal is accessing multiple levels of the cervical spine.Payments/cost
San Francisco posterior cervical laminoplasty patients pay an average of $17,734 for this procedure. However, spinal surgery can cost upward of $100,000 easily if a patient does not have insurance.This is the name for the procedure performed from the back to alleviate pressure on nerves which are compressed from stenosis. The back part of the spine, the lamina, is opened and the compression is decreased. The bone may be secured in the new, opened position with bone or plates and screws.
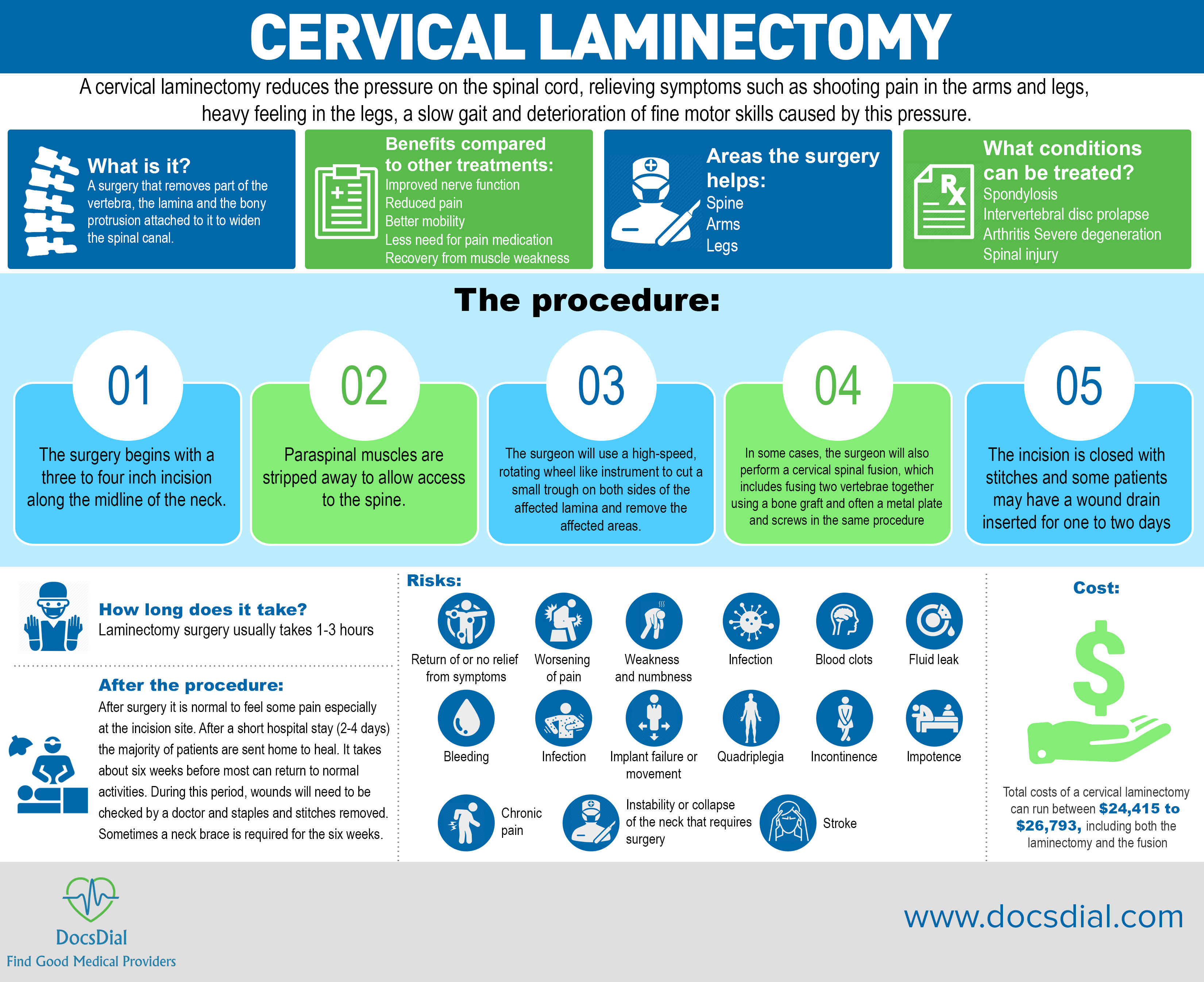
Posterior cervical Laminectomy and fusion
Eliminate back pain in San Francisco through laminectomy and fusion surgery.
75% of San Francisco back pain patients who suffer spinal cord compression and/or myelopathy see a significant improvement in symptoms.
 For those who suffer from cervical spinal stenosis, a narrowing of the spinal canal commonly caused by age-related changes to the spine, spondylosis or an intervertebral disc prolapse, a cervical laminectomy may provide relief. Those with arthritis or severe degeneration, or those who have experienced trauma may benefit from having a fusion as part of the procedure, as well.
For those who suffer from cervical spinal stenosis, a narrowing of the spinal canal commonly caused by age-related changes to the spine, spondylosis or an intervertebral disc prolapse, a cervical laminectomy may provide relief. Those with arthritis or severe degeneration, or those who have experienced trauma may benefit from having a fusion as part of the procedure, as well.
What is it?
A San Francisco cervical laminectomy reduces the pressure on the spinal cord, relieving symptoms such as shooting pain in the arms and legs, heavy feeling in the legs, a slow gait and deterioration of fine motor skills caused by this pressure. During the surgery, part of the vertebra, the lamina and the bony protrusion attached to it are removed. Before surgery, take steps to increase your chances of a positive outcome. These steps are based on the individual but often include changing medications, stopping smoking and losing weight. Dr. Abbi may recommend a protocol of zinc tablets before and after surgery to promote wound healing. Dr. Abbi won’t recommend surgery unless other interventions have failed and proper tests have been done. These tests include x-rays, CTs and MRIs to provide a better look at the cervical spine. If imaging is inconclusive, nerve conduction studies and/or a nerve block may be used to provide better answers. Cervical laminectomy surgeries in San Francisco are performed under general anesthesia and a breathing tube will be put in to protect the airway during surgery. To prevent infection and nausea, medicine will be given intravenously, as well. Local anesthetic is also used to treat the area the incision will be made. After surgery it is normal to feel some pain especially at the incision site. Most patients are on their feet within a few hours or the procedure. After a short hospital stay (2-4 days) the majority of patients are sent home to heal. It takes about six weeks before most can return to normal activities. During this period, wounds will need to be checked by a doctor and staples and stitches removed. Sometimes a neck brace is required for the six weeks.Purpose
The purpose of cervical laminectomy is to reduce or eliminate symptoms caused by cervical spine stenosis when other interventions have failed, which is done by relieving pressure or pinched nerves in the cervical spine. With fusion, the spine can also be stabilized, which is often necessary if more than one vertebrae has been affected. Most patients notice relief from pain, aching, stiffness, numbness, tingling sensations and weakness in the neck and other parts of the body. The main symptom cervical laminectomy improves is pain, especially in the arm. Other symptoms including pain in the neck, headaches, numbness and weakness may or may not improve with surgery.Benefits
San Francisco patients who undergo a cervical laminectomy typically report less pain as well as reduction or elimination from other symptoms stemming from a reduced tunnel for the spinal cord and nerve roots to pass through. Patients also typically have improved nerve function and the surgery can prevent abnormal motion in the spine as well as further deterioration by relieving pressure on the spine and its nerves. Many patients are able to reduce the amount of medication they take after surgery, as well. Stabilization of the spine is possible, especially when fusion is done as part of the procedure. Patients from San Francisco with arm pain and muscle weakness usually recover best while neck pain and headaches may or may not improve, with a small number of cases reporting worsening of these symptoms post surgery. If damage has already been done to the spinal cord and spinal nerves, symptoms of numbness and balance may not improve either. If you don’t experience a relief of numbness immediately, don’t fret. That symptom can take up to 12 months to really improve. Without treatment, however, persistent pain, paralysis, weakness, numbness, functional impairment problems with walking and balance are common.Areas the Surgery Helps:
San Francisco cervical laminectomy and fusion surgery relieves pain in the arms, legs and spine.What conditions can be treated?
San Francisco spondylosis, intervertebral disc prolapse, arthritis, severe degeneration and spinal injury patients find relief with cervical laminectomy and fusion surgery.The procedure:
Laminectomy surgery usually takes 1-3 hours.- The surgery begins with a three to four inch incision along the midline of the neck.
- Paraspinal muscles are stripped away to allow access to the spine.
- The surgeon will use a high-speed, rotating wheel like instrument to cut a small trough on both sides of the affected lamina and remove the affected areas.
- In some cases, the surgeon will also perform a cervical spinal fusion, which includes fusing two vertebrae together using a bone graft and often a metal plate and screws in the same procedure
- The incision is closed with stitches and some patients may have a wound drain inserted for one to two days
Risks
Major complications are not common during cervical laminectomy. The rate of minor complications is also low; with three or four out of every 100 patients experiencing a minor complication. Risks of the surgery include return of or no relief from symptoms, worsening of pain, weakness and numbness, infection, a blood clot, fluid leak, blood loss that could lead to an infection, implant failure or movement, quadriplegia, incontinence, impotence, chronic pain, instability or collapse of the neck that requires surgery and stroke. General anesthesia carries its own risks including death, drug allergy, pulmonary embolism and infection, but most of these complications are rare.After the Procedure
After San Francisco cervical laminectomy and fusion surgery it is normal to feel some pain especially at the incision site. After a short hospital stay (2-4 days) the majority of patients are sent home to heal. It takes about six weeks before most can return to normal activities. During this period, wounds will need to be checked and staples and stitches removed. Sometimes a neck brace is required for the six weeks.Alternatives
Before surgery is recommended, most patients undergo other treatments including: pain medication, nerve sheath injections in the compressed nerves to relieve pain, modification of activities, physiotherapy, osteopathy, hydrotherapy and massage. Other surgical procedures are also an option. Ask your doctor about artificial disc replacement, foraminotomy and anterior cervical decompression and fusion (ACDF).Payments/cost
Total costs of a San Francisco cervical laminectomy can run between $24,415 to $26,793, including both the laminectomy and the fusion. It is not uncommon for the total cost of diagnosing, treating and recovering from spinal surgery to cost $100,000 before insurance. If you have insurance, it will often cover some or all of the procedure so check with your provider for an estimate. Don’t forget to factor in other expenses, including a neck brace, post-surgery care and physical therapy.References:
Burke, Stephanie. "A Step-by-Step Guide to Cervical Laminectomy Surgery." Spine-health. Accessed May 03, 2018. https://www.spine-health.com/blog/how-cervical-laminectomy-surgery-helps-relieve-pressure. "Cervical Laminectomy and Fusion." How Much Does a Cervical Laminectomy and Fusion Cost? What Is a Cervical Laminectomy and Fusion? - MDsave. Accessed May 03, 2018. https://www.mdsave.com/procedures/cervical-laminectomy-and-fusion/d482fdcc. "Cervical Laminectomy Spine Treatment | Neurosurgery." Precision Brain, Spine & Pain Centre. Accessed May 03, 2018. https://www.precisionhealth.com.au/healthcare-services/advanced-neurosurgery-spinal-surgery/procedures-and-surgery/cervical-laminectomy/.This is the name for the procedure performed from the back to alleviate pressure on nerves which are compressed from arthritis. The back part of the spine, the lamina, is removed in part or completely, and the extra soft tissue that has overgrown and compressing the nerves is removed. Since removal of this bone can weaken the structure of the spine, a fusion is then done with screws and rods to strengthen the spine and to decrease pain.
Lumbar Laminectomy
San Francisco back pain sufferers – Eliminate back pain with a Lumbar Laminectomy & Fusion surgery. 80% of San Francisco back pain patients who undergo a successful laminectomy, significantly reduce back pain and the underlying issues that cause it. During a San Francisco lumbar laminectomy, a spinal surgeon removes pressure on spinal nerves in the lumbar spine (lower back) by opening the spinal canal and making it larger. In a posterior procedure this is done through an incision made in the patient’s back. As a result, the nerves in the lumbar spine that pass through the spinal cord are protected and the pain caused by degenerative changes in the invertebral discs of the lumbar spine and the joints in that region is lessened. Literally laminectomy translates to “remove the lamina” (the back side of the spinal canal that forms the roof over the spinal cord).
What is it?
Degenerative disc disease can lead to spinal stenosis, when the invertebrae and bone spurs within the invertebrae put pressure on the spinal nerves. With spinal stenosis the only way to relieve back pain for San Francisco sufferers is to widen the spinal canal and remove any bone spurs putting pressure on the spinal nerves. This is done during a laminectomy. As a result the spinal nerves are no longer irritated and swelling will go down leading to a decrease in back pain. Before surgery an x-ray is done to identify which vertebrae are causing the issues in the back. These are the ones Dr. Abbi will target during surgery. In some cases a San Francisco lumbar laminectomy are done as minimally invasive surgeries. In this case the surgeon will make a few small incisions to access the spine and use small tools to remove damaged lamina and bone spurs. This saves patients the large incision used in an open procedure as well as many risks associated with open procedures. However, not every patient is a candidate for a minimally invasive spine surgery. If much of the facet joints are removed during surgery then a fusion will be done during the operation to ensure the spine’s integrity. During a fusion the vertebrae are fused together. This prevents motion in the area between the two vertebrae but it also increases stability in the region. An instable spine is susceptible to several problems later in life. After San Francisco lumbar laminectomy surgery it can take weeks or even months to heal. Rehabilitation programs will help patients strengthen their backs but back pain patients in San Francisco should assume they will not be able to drive for two weeks and may need strong medications to get by in the beginning. Patients may also need to make adjustments while showering and bathing to keep the incision site clean and dry.Purpose
The purpose of a lumbar laminectomy is to alleviate back pain in the lumbar (or lower) spine by relieving pressure on the spinal nerves caused by spinal stenosis. When a fusion is done as part of a laminectomy the goal is to offer increased stability in the spine and prevent future problems in that area. For many, spine surgery is a life-changing operation; one that returns them to normal daily life with reduced pain or completely relieved of back pain in the targeted area.Benefits
The largest benefit of undergoing a lumbar laminectomy in San Francisco is reduced or completely eliminated lower back pain. With a minimally invasive procedure there are additional benefits, including faster healing and reduced risk of infection. Scars are also smaller and often less visible. A San Francisco lumbar laminectomy is completed in order to relieve a patient of significant lower back pain caused by pressure on the spinal nerves. When fusions are done as part of a lumbar laminectomy, stability is often also improved. This can create better posture and ease of performing daily tasks. Some patients may be able to ditch their walkers, canes or other assistive walking devices after surgery.Areas the Surgery Helps:
San Francisco lumbar laminectomy surgery reduces or eliminates knee and leg pain.What conditions can be treated?
San Francisco lumbar laminectomy surgery treats degenerative disc disease, spinal stenosis and severe back pain.The procedure:
How long a San Francisco lumbar laminectomy takes depends on how many vertebrae need to be treated and whether or not the procedure is open or minimally invasive.- An x-ray is done to identify the vertebrae causing the pain.
- The patient will be given general anesthesia.
- An incision (or several small incisions) is made down the center of the back and the muscles are moved aside so the surgeon can access the spine.
- The lamina are removed on the problem vertebrae as well as any bone spurs putting pressure on the spinal nerves.
- Once the small amount of bone has been removed, it is then possible to remove the herniated disc and other soft tissues around the nerve.
- The patient will undergo a fusion as well if needed.
- The patient is closed using sutures and staples and wheeled to recovery.
Risks
As with every surgery there are risks, and spinal surgeries can be especially risky for some patients. Additional pain or even paralysis can occur because surgeons are working so close to the spinal cord. Several types of injury to the spinal cord, in fact, are possible. In some patients pain relief is not significant and numbness, tingling and significant pain post-operation can happen. Difficulty breathing and other lung problems can also arise. In some cases the hardware inserted during surgery can fracture or hardware can migrate to an area of the body where it does not belong requiring subsequent surgeries. There are other risks associated with general anesthesia and incisions such as a serious reaction to the drugs or infection in the wound. As with any surgery that keeps you immobile for a period of time a patient can develop blood clots, or DVT. Those in poor health or elderly patients face increased risks. For a complete list of possible complications, consult Dr. Abbi.After the procedure:
Significant pain is common post-surgery and the San Francisco back pain patient will likely spend a few days in the hospital. Physical therapy as well as pain medication will be prescribed and Dr. Abbi will get patients up and moving as soon as possible to limit post-surgical risks. With a fusion, patients can expect recovery to take 2-4 months. Without a fusion a patient should be performing many normal tasks in about two weeks.Alternatives
There are several types of back surgery that can be done to relieve back pain for San Francisco patients in the lumbar spine for. Before surgery is recommended, other interventions such as physical therapy or pain medication are often tried. The procedure outlined in this article covers both open and minimally invasive approaches. Some surgeons may suggest alternative approaches in a similar surgery. A lumbar laminectomy is, however, one of the most popular types of back surgery completed in the U.S.Payments/Cost
Without health insurance a lumbar laminectomy can cost anywhere from $50,000-90,000 on average. However, for those with medical insurance, the insurance company should cover a significant portion of the procedure leaving San Francisco back pain patients to pay between $200-2,000 on average, plus any deductible that needs to be met.References:
Lumbar Laminectomy. (n.d.). Retrieved from https://www.umms.org/ummc/health-services/orthopedics/services/spine/patient-guides/lumbar-laminectomy Getting a Laminectomy: Before, During, and After. (n.d.). Retrieved from https://www.webmd.com/back-pain/guide/laminectomy-surgery-before-during-and-after#2-4 How Much Does Back Surgery Cost? - CostHelper.com. (n.d.). Retrieved from http://health.costhelper.com/back-surgery.htmlA microdiscectomy is the specific name for the procedure to alleviate pressure on nerves which are compressed due to a disc herniation. The procedure involves removing a small amount of bone to allow access to the spinal canal. The bone that is removed is not important for the structural support of the spine so removing this bone does not lead to instability or dysfunction. Once the small amount of bone has been removed, it is then possible to remove the herniated disc and other soft tissues around the nerve. The remainder of the disc is left in place to provide motion and stability.
Lumbar Spinal Fusion
Up to 90% of patients experience pain relief with San Francisco Lumbar Spinal Fusion.
Pain after TLIF specifically is reduced 60-70 percent on average.
A San Francisco lumbar spinal fusion is a type of back surgery that can be done as an open, minimally invasive or mini-open procedure.
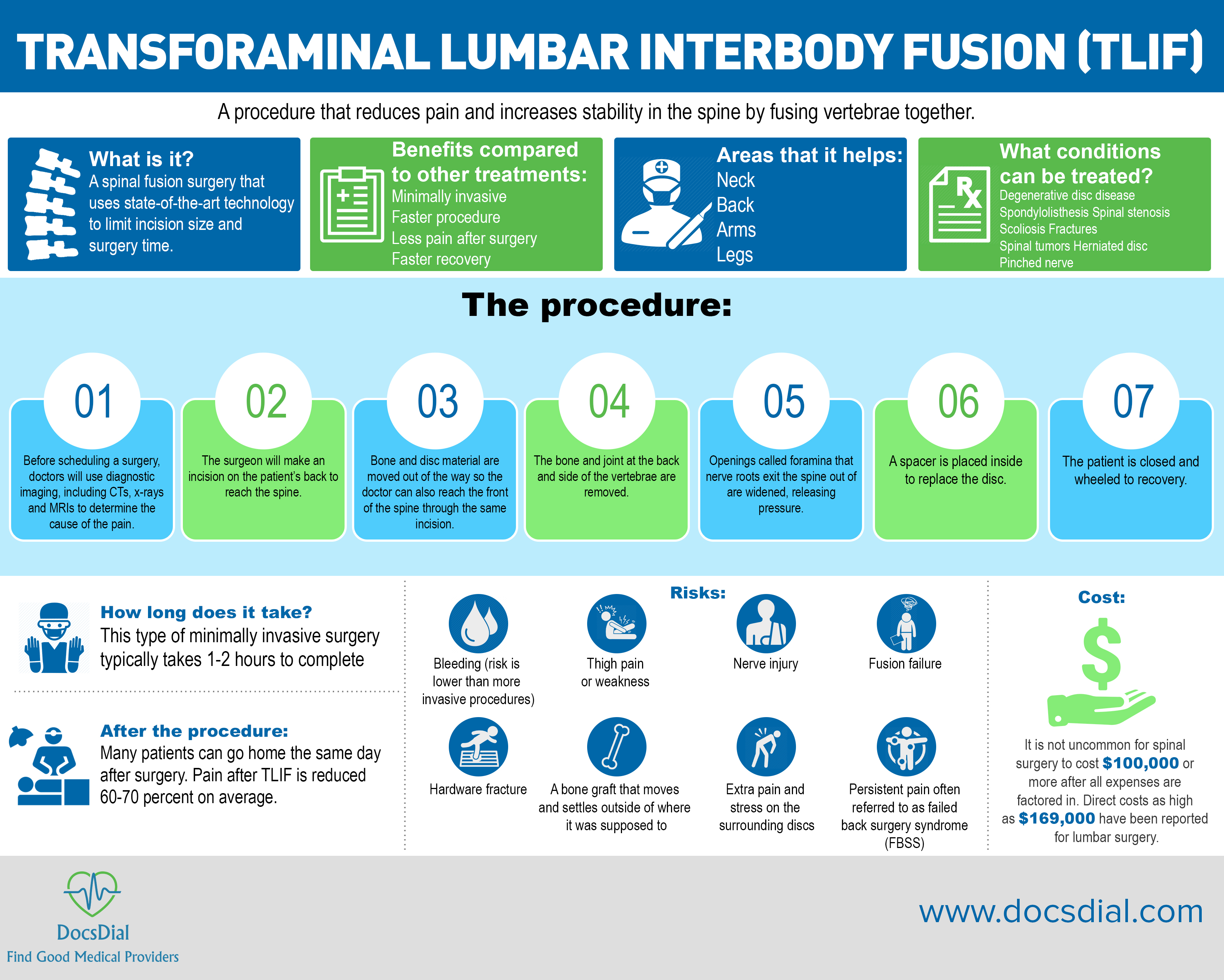 The procedure combines two or more vertebrae through a welding-like process in order to reduce pain and increase stability in the spine. It is used to treat chronic neck and back pain that may radiate to the arms and legs. People who suffer conditions such as degenerative disc disease, spondylolisthesis, spinal stenosis, scoliosis, fractures and spinal tumors in San Francisco typically make good candidates for the procedures. When possible, some spinal fusion surgeries can be done as outpatient procedures with minimal cutting and operating time—they are called minimally invasive spinal fusions. Depending on which vertebrae are causing pain and where potentially diseased discs are located, a fusion can be done on the thoracic (upper back) or lumbar spine (lower back).
The procedure combines two or more vertebrae through a welding-like process in order to reduce pain and increase stability in the spine. It is used to treat chronic neck and back pain that may radiate to the arms and legs. People who suffer conditions such as degenerative disc disease, spondylolisthesis, spinal stenosis, scoliosis, fractures and spinal tumors in San Francisco typically make good candidates for the procedures. When possible, some spinal fusion surgeries can be done as outpatient procedures with minimal cutting and operating time—they are called minimally invasive spinal fusions. Depending on which vertebrae are causing pain and where potentially diseased discs are located, a fusion can be done on the thoracic (upper back) or lumbar spine (lower back).
What is it?
San Francisco spinal fusions prevent pain associated with movement by fusing together two or more vertebrae in the spine to prevent painful movement. The pieces are welded together using a bone graft, made from either a cadaver bone or taken from the patient. These grafts are commonly referred to as cages. To be effective, Dr. Abbi has to be able to tell which vertebrae are causing the problems, so before scheduling a surgery they will use diagnostic imaging, including CTs, x-rays and MRIs to determine the cause of the pain. Without this knowledge, a spinal fusion is not typically recommended. There are two types of minimally invasive spinal fusions that target the lumbar spine—transforaminal lumbar interbody fusion, or TLIF, and lateral lumbar interbody fusion, called LLIF or XLIF. A transforaminal lumbar interbody fusion is used when Dr. Abbi needs to access both the front and back of the spine during the procedure. In addition to fusing the bones together with a bone graft, the surgery decompresses the spinal cord and/or spinal nerves and provides stability to the spine. There are several levels to this surgery. The first is called an open procedure and is not minimally invasive. There is also a minimally invasive version that uses smaller incisions and instruments to access the spine through, offering benefits including less pain post-surgery and shorter recovery times. In between these two approaches is the mini-open, which uses some of the minimally invasive techniques but not all of them, offering a middle ground in cases where a true minimally invasive surgery cannot be done. The other procedure—the lateral lumbar interbody fusion—uses a one-inch incision in the side of the waist to achieve the spinal fusion. After the damaged disc is removed, Dr. Abbi replaces it with a bone graft that acts as a spacer and helps the bone fuse together. If instability is of major concern, the surgeon may place a plate and screws into the spine as well to hold the spine steady and promote healing. In some cases an additional incision is made from the back (posterior) to insert stabilizing equipment. The surgery is performed by a neurosurgeon or orthopedic surgeon with special training in minimally invasive surgery and typically takes 1-2 hours to complete.Purpose
The main purpose of lumbar fusion is to reduce pain and create more stability in the spine. There are many options for San Francisco back pain sufferers. LLIF and TLIF is to reduce or eliminate pain in San Francisco back, arm and/or leg pain sufferers caused by movement in the spine. It was created as a minimally invasive alternative to other spinal fusion surgeries. With its smaller incision there is less potential for damage of nerves, blood vessels and organs. In an LLIF, instead of using normal instruments, tubular instruments are passed through the small space using a tunnel formed by the surgeon between the patient's abdominal organs and the spine muscles. In the TLIF, both parts of the spine are able to be worked on from one incision eliminating additional risks and a second incision site that can cause post-operative pain. Many patients prefer the lateral or transforminal approach to anterior or posterior interbody fusion procedures because they can go home the same day and recovery is shorter. Open and mini-open procedures find the same results for patients with a different approach. Dr. Abbi will recommend the best procedure for you.Benefits
The biggest benefit of San Francisco lumbar fusion surgery is pain relief. Whether it is complete or partial, most patients experience improvement in pain as well as becoming better able to perform daily tasks due to the reduction in pain. In most cases, patients do not notice the limited movement caused by fusion because they couldn’t move without pain before. This pain is commonly caused by other ailments that affect the spine such as a pinched nerve, degenerative disc disease, degenerative scoliosis or a herniated disc. Most patients report lower pain levels post surgery, as well as the ability to function better in daily life and perform normal activities. Other benefits include correcting mild to moderate scoliosis, relieving radiating pain and sensations such as numbness, weakness or tingling in the arms and legs, less stiffness upon walking or standing and being able to go home the same day as surgery thanks to the minimally invasive outpatient procedure. Minimally invasive surgery often causes less tissue trauma, less scarring and less postoperative discomfort, plus it requires shorter hospital stays.Areas the Surgery Helps:
San Francisco lumbar fusion surgery relieves pain in the lumbar spine, neck, back, arms and legs.What conditions can be treated?
San Francisco lumbar fusion surgery helps those who suffer degenerative disc disease, spondylolisthesis, spinal stenosis, scoliosis, fractures and spinal tumors.The procedure:
Lumbar fusion surgery can take anywhere from 2.5-7 hours often depending on how many levels of fusion must be done. The minimally invasive version takes 1-2 hours.- Before scheduling surgery, Dr. Abbi will use imaging machines to determine which vertebrae to operate on.
- The patient will be given general anesthesia before the procedure.
- Abbi will make an incision on the patient’s back to reach the spine
- In minimally invasive procedures, bone and disc material are moved out of the way so the doctor can also reach the front of the spine through the same incision. In open procedures a second incision will be made from the front.
- Abbi removes the bone and joint at the back and side of the vertebrae.
- Abbi widens the foramina that nerve roots exit through.
- A spacer is placed inside to replace the removed disc.
- Bone grafts or metal plates are used to fuse the spine together.
- The patient is closed and wheeled to recovery.
Risks
Every surgery includes the following risks: bleeding, infection, blood clots and reactions to anesthesia. Lateral lumbar interbody fusion and transforaminal lumbar interbody fusion have their own risks, but they are limited due to the small incision and short operating time. Bleeding, especially, is of less concern. Other complications include: thigh pain or weakness that lasts weeks to months, nerve injury, abdominal organ injury (LLIF), fusion failure (meaning the graft didn’t effectively fuse the vertebrae into one bone), hardware fracture, a bone graft that moves and settles outside of where it was supposed to, extra pain and stress on the surrounding discs and persistent pain often referred to as failed back surgery syndrome, or FBSS.After the procedure:
Patients should anticipate some pain following San Francisco lumbar fusion surgery, and it can take 3-12 months for a full recovery. After the procedure patients should undergo physical therapy to regain strength and range of motion as well as schedule a follow-up appointment 4-6 weeks after.Alternatives
Back surgery is almost never recommended unless other methods have failed first. Before resorting to even this minimally invasive procedure, Dr. Abbi will try a mix of other interventions including pain medication, physical therapy, other physical modalities possibly including massage or acupuncture and sometimes steroid shots in the spine to relieve pain. If lumbar fusion is needed, there are several types of spinal fusions available. LLIF and TLIF are often preferred for their small incisions and short operating times but they aren’t always a good fit for candidates. Instead, anterior lumbar interbody fusion, posterior lumbar interbody fusion or another type of spinal fusion surgery may be recommended to treat vertebrae and damaged discs in the lumbar spine.Payments/cost
It is not uncommon for spinal surgery to cost $100,000 or more after all expenses are factored in—the surgery, recovery, physical therapy, diagnostic imaging, medication and disability. Direct costs as high as $169,000 have been reported for lumbar surgery. Where you have the surgery and who performs it will also affect cost. Insurance, luckily, often covers all or part of the surgery. Check with your provider for an accurate estimate, and don’t forget to factor in aftercare.References:
"Back Surgery: Too Many, Too Costly and Too Ineffective." Common Exercise Mistakes. June 01, 2011. Accessed May 05, 2018. http://www.toyourhealth.com/mpacms/tyh/article.php?id=1447. "Spinal Fusion: Lateral Lumbar Interbody Fusion (LLIF)." , Hemorrhagic Stroke. Accessed May 05, 2018. https://www.mayfieldclinic.com/pe-llif.htm. "Lateral Lumbar Interbody Fusion (XLIF) Video." Spine-health. Accessed May 05, 2018. https://www.spine-health.com/video/lateral-lumbar-interbody-fusion-xlif-video. Laser Spine Institute. "Lateral Lumbar Interbody Fusion | Minimally Invasive Stabilization (MIS) Options for Lumbar Spine." Laser Spine Institute. Accessed May 05, 2018. https://www.laserspineinstitute.com/spinal_orthopedic_procedures/llif/. Montgomery, Stephen P. "TLIF Back Surgery Success Rates and Risks." Spine-health. Accessed May 05, 2018. https://www.spine-health.com/treatment/spinal-fusion/tlif-back-surgery-success-rates-and-risks. Mudbug. "Spinal Fusion: Do You Really Need One?" Michael A. Gleiber, MD. April 20, 2015. Accessed May 05, 2018. https://michaelgleibermd.com/news/really-need-spinal-fusion/. Transforaminal Lumbar Interbody Fusion (TLIF) – The Spine Hospital at The Neurological Institute of New York." The Spine Hospital at The Neurological Institute of New York. Accessed May 05, 2018. http://columbiaspine.org/treatments/transforaminal-lumbar-interbody-fusion-tlif/Fusion is a surgical technique in which one or more of the vertebrae of the spine are united together (“fused”) so that motion no longer occurs between them.The lack of motion helps to decrease the back pain. Bone grafts are placed around the spine during surgery. The body then heals the grafts over several months – similar to healing a fracture – which joinsthe vertebrae together. Spinal fusion can help in the correction of deformity (spinal curves) the treatment of instability (spondylolisthesis) or management of painful intervertebral discs (degenerative disc disease). A spinal decompression is a procedure to remove pressure form compressed (pinched) nerves. This includes removing bone or soft tissue that is causing the pressure on the nerves. Once all the compressed nerves are alleviated of compression, the leg pain usually improves. This removed bone is then used as the bone graft to help the spinal fusion. This procedure (called laminectomy) is often done together with a fusion.
Knee replacement
 San Francisco knee and hip pain sufferers – Eliminate pain with a Total Knee Replacement.
90% of San Francisco knee pain patients report significantly reduced pain after surgery.
85% of artificial knees last 20+ years.
San Francisco knee and hip pain patients undergo a TKR if they have arthritis in the hip that has not resolved with conservative treatment.
Candidates for San Francisco total knee replacement surgeries aren’t just looking to relieve a little pain. While pain relief is a main reason for the surgery, those who need a full replacement often have structural deformities such as bowed legs or knocked knees due to bone loss, and the deformity is often very noticeable. When this happens, it’s harder to move the knees without pain and there can be significant loss of motion. Grinding and severe pain are among chief complaints of those who need total knee replacement surgery.
San Francisco knee and hip pain sufferers – Eliminate pain with a Total Knee Replacement.
90% of San Francisco knee pain patients report significantly reduced pain after surgery.
85% of artificial knees last 20+ years.
San Francisco knee and hip pain patients undergo a TKR if they have arthritis in the hip that has not resolved with conservative treatment.
Candidates for San Francisco total knee replacement surgeries aren’t just looking to relieve a little pain. While pain relief is a main reason for the surgery, those who need a full replacement often have structural deformities such as bowed legs or knocked knees due to bone loss, and the deformity is often very noticeable. When this happens, it’s harder to move the knees without pain and there can be significant loss of motion. Grinding and severe pain are among chief complaints of those who need total knee replacement surgery.
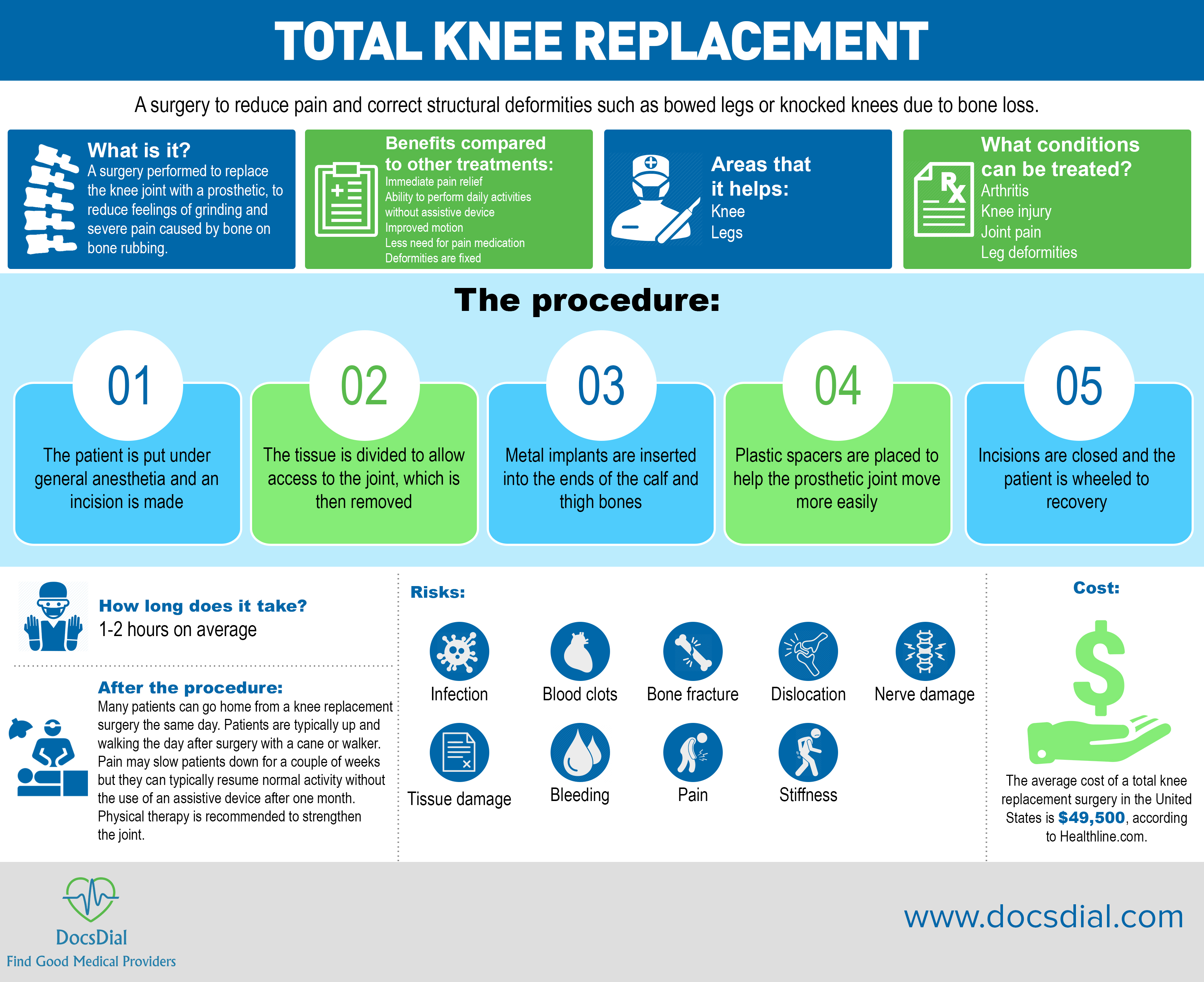
What is it?
 San Francisco knee replacement surgery typically takes one to two hours to complete. During this time, damaged bone and cartilage are taken out of the knee and metal implants are inserted into the ends of the calf and thigh bones. Plastic spacers are used to help the prosthetic joint move more easily.
New technologies have changed the way many doctors do knee surgery and given surgeons more options on how to complete the procedure. Computer-aided surgeries, for example, are becoming more common in knee surgeries. The technology has been praised for allowing better placement of the new joint, which helps the new joint last longer. It can also be more beneficial in surgeries where deformities are extreme. When a knee joint is inserted correctly it is less likely to loosen early or wear down quickly.
Not every doctor says the computer-aided technology is an improvement, as knee replacements were already a pretty routine procedure at most hospitals, but the new technology does allow for a new approach that could include some improvements in recovery for the patient.
Many San Francisco total knee replacements can now be done as outpatient procedures, which means a patient goes home the same day as the operation. By prescribing fewer narcotics post-operatively, San Francisco knee pain and hip pain patients are able to get up and move around sooner, which leads to less complications and a faster recovery. Pain may slow patients down for a couple of weeks, but it doesn’t take long for the pain to subside, and then patients feel better than they did before the procedure. With new protocols in place, patients are typically up and walking the day after surgery with a cane or walker, home in one to two days (if the procedure isn’t done outpatient) and resuming normal activity without the use of an assistive device after one month.
San Francisco knee replacement surgery typically takes one to two hours to complete. During this time, damaged bone and cartilage are taken out of the knee and metal implants are inserted into the ends of the calf and thigh bones. Plastic spacers are used to help the prosthetic joint move more easily.
New technologies have changed the way many doctors do knee surgery and given surgeons more options on how to complete the procedure. Computer-aided surgeries, for example, are becoming more common in knee surgeries. The technology has been praised for allowing better placement of the new joint, which helps the new joint last longer. It can also be more beneficial in surgeries where deformities are extreme. When a knee joint is inserted correctly it is less likely to loosen early or wear down quickly.
Not every doctor says the computer-aided technology is an improvement, as knee replacements were already a pretty routine procedure at most hospitals, but the new technology does allow for a new approach that could include some improvements in recovery for the patient.
Many San Francisco total knee replacements can now be done as outpatient procedures, which means a patient goes home the same day as the operation. By prescribing fewer narcotics post-operatively, San Francisco knee pain and hip pain patients are able to get up and move around sooner, which leads to less complications and a faster recovery. Pain may slow patients down for a couple of weeks, but it doesn’t take long for the pain to subside, and then patients feel better than they did before the procedure. With new protocols in place, patients are typically up and walking the day after surgery with a cane or walker, home in one to two days (if the procedure isn’t done outpatient) and resuming normal activity without the use of an assistive device after one month.
Purpose
 Those who undergo total knee replacements in San Francisco notice a significant, immediate change in pain. In many cases, a total knee replacement surgery can also fix a deformity, or at least lessen its affect. Daily activities become easier to complete because of reduced pain, and that grinding/grading feeling many patients complain about can be eliminated. Range of motion may never return to what it was before the knee started experiencing problems, but it should be improved with the possibility of complete recovery in some cases.
Those who undergo a total knee replacement in San Francisco report a reduction in pain, or complete elimination of pain, fixed deformities such as knocked knees or bowed legs, no more grinding or grading feeling caused by the bones within the joint rubbing against each other and the ability to do day to day activities without pain or the use of assistive devices.
Those who undergo total knee replacements in San Francisco notice a significant, immediate change in pain. In many cases, a total knee replacement surgery can also fix a deformity, or at least lessen its affect. Daily activities become easier to complete because of reduced pain, and that grinding/grading feeling many patients complain about can be eliminated. Range of motion may never return to what it was before the knee started experiencing problems, but it should be improved with the possibility of complete recovery in some cases.
Those who undergo a total knee replacement in San Francisco report a reduction in pain, or complete elimination of pain, fixed deformities such as knocked knees or bowed legs, no more grinding or grading feeling caused by the bones within the joint rubbing against each other and the ability to do day to day activities without pain or the use of assistive devices.
Benefits
The benefits of San Francisco total knee replacement surgeries include reduced pain and the ability to complete daily activities pain-free, or relatively pain-free, without the use of assistive devices. Those who undergo a total knee replacement will find it easier to sit, stand and lay down without pain. Deformities such as bowed legs or knocked knees, which affect gait, can be righted.Areas the Surgery Helps:
San Francisco TKR surgery reduces or eliminates knee, hip and leg pain.What conditions can be treated?
San Francisco TKR surgery treats arthritism knee injury, joint pain and leg deformities.The procedure:
San Francisco TKR surgery takes 1-2 hours on average to complete.- The patient is put under general anesthesia and an incision is made
- The tissue is divided to allow access to the joint, which is then removed
- Metal implants are inserted into the ends of the calf and thigh bones
- Plastic spacers are placed to help the prosthetic joint move more easily
- Incisions are closed and the patient is wheeled to recovery
After the procedure:
 Many patients can go home from a knee replacement surgery the same day. Patients are typically up and walking the day after surgery with a cane or walker. Pain may slow patients down for a couple of weeks but they can typically resume normal activity without the use of an assistive device after one month. Physical therapy is recommended to strengthen the joint.
Many patients can go home from a knee replacement surgery the same day. Patients are typically up and walking the day after surgery with a cane or walker. Pain may slow patients down for a couple of weeks but they can typically resume normal activity without the use of an assistive device after one month. Physical therapy is recommended to strengthen the joint.
Alternatives
Before knee surgery, many people try to manage knee pain in San Francisco with medication and/or cortisone shots. Some doctors are suggesting that stem cell injections could repair joints enough that surgery would not be needed. Other interventions can reduce pain in the knee such as physical therapy, losing weight and exercising to strengthen the muscles and increase flexibility. In some cases, a partial knee replacement—which costs 10-20 percent less than a total knee replacement—may suffice and a total knee replacement can be avoided.Risks
There are risks associated with every surgery, and often those risks are made worse by underlying health issues. For example, a patient who is obese is at a higher risk of suffering complications during surgery, and their weight could make their recovery more difficult. A history of heart disease, diabetes or depression can also affect how well a person fairs during surgery and recovery. Mostly these conditions extend the healing process but they do also increase the risk of surgery itself. If you have underlying disease, talk it over with your doctor. If the procedure is too risky, they’ll advise against it, however, that is rare in most cases for knee replacement surgery. Before a total knee replacement surgery, every San Francisco knee pain patient should take steps to make the procedure go more smoothly such as lose weight or quit smoking. Knocking bad habits and improving overall health can also make recovery easier and faster. Risks associated with general anesthesia should also be discussed with your doctor.Payments/cost
The average cost of a total knee replacement surgery in the United States is $49,500, according to Healthline.com. Luckily, insurance will often cover all or part of a total knee replacement, lowering the out-of-pocket cost for patients. Dr. Abbi performs the procedure in San Francisco and surrounding cities.References:
"OA Knee Replacement Pictures: Before and After -- What Happens?" WebMD. Accessed April 23, 2018. https://www.webmd.com/osteoarthritis/ss/slideshow-knee-replacement. HARITINIAN, Emil G., and Ashvin L. PIMPALNERKAR. "Computer Assisted Total Knee Arthroplasty: Does It Make a Difference?" Mædica. June 2013. Accessed April 23, 2018. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3865127/. "Alternatives to Knee Replacement Surgery." Healthline. Accessed April 23, 2018. https://www.healthline.com/health/total-knee-replacement-surgery/alternatives. "What You Need to Know About the Cost of Knee Replacement Surgery." Healthline. Accessed April 23, 2018. https://www.healthline.com/health/total-knee-replacement-surgery/understanding-costsTotal knee replacement is indicated if you have arthritis in the hip and have failed conservative measures. For more information click here: http://orthoinfo.aaos.org/topic.cfm?topic=A00389
Fracture care
San Francisco broken bone sufferers—get quality fracture care close to home! 100% of broken bones can be fixed. Fracture care refers to several modalities and approaches used to treat bone fractures caused by overuse, injury or osteoporosis. There are several different types of bone fractures:
- Open or compound fracture
- Stable fracture
- Transverse fracture
- Oblique fracture
- Comminuted fracture

What is it?
Fracture care includes many different approaches to treating all kinds of fractures. Every care plan starts with an examination by a doctor so the fracture can be assessed and diagnosed. The type of fracture you have determines care. Some of the more common care options include:- Casts or braces
- Traction
- External fixation
- Internal fixation
- Open reduction
Purpose
Fracture care is a series of interventions that are used to treat and heal bone fractures throughout the body. Dr. Abbi offers several options for fracture care including two surgical options, internal fixation and open reduction, which are used to treat more serious fractures.Benefits
Fracture care relieves pain in patients who suffer from broken bones by setting and healing the bones back in place. In many cases it is a lengthy process to heal broken bones, but a mix of interventions can be used to achieve the best results. The biggest benefits are pain relief, healed bones and better movement/function in the affected area.Areas the surgery helps:
Surgery and non-surgical fracture care options treat bone fractures throughout the body.What conditions can be treated?
San Francisco fracture care reverses and heals bone fractures caused by osteoporosis, injury or overuse.The procedure:
The length of surgery depends on what type of fracture being fixed and how bad the fracture is. Bones that are fractured in multiple places typically take longer to treat. Each care option has its own procedure. Casting and braces are pretty straight forward. The open reduction and internal fixation are the only surgical procedures on the list. Here is the process:- The patient is placed under general anesthesia.
- Abbi makes incisions to access the part of the bone that has fractured.
- Abbi will reposition the bones in the correct position to promote proper healing.
- Screws or metal plates will be attached to the bone to hold it in the correct position as it heals. Sometimes rods are used instead.
- The patient is closed and wheeled to recovery.
Risks:
Every surgery carries risks. Often risk factors are made worse by other modalities. Unhealthy patients who are overweight or have bad habits such as smoking or excessive drinking are at higher risk for complications during surgery. Because this procedure requires general anesthesia, patients should be aware of the risks associated with that drug, which include death, stroke, deep vein thrombosis, pulmonary embolism and drug allergy. Other risks associated with San Francisco fracture care are infection, blood loss, nerve damage, pain from screws/equipment, movement of equipment, bacterial colonization of the bone, loss of motion, stiffness, muscle damage, arthritis, palsy, nonunion and tendonitis.After the procedure:
It can take weeks or even months for any bone fracture to heal. The more severe the fracture, the longer and typically more painful the recovery is. Continue to visit your doctor to determine how much activity your bone can handle and to manage pain if it persists. Physical therapy may be recommended after to promote strengthening and better movement.Cost:
The cost of a cast varies but patients can expect to pay an average of $500. The cost of ORIF surgery also varies depending on the bone being treated. Patients can expect to pay anywhere from $3,000-$7,000.For information about options for fracture treatment, click here: http://orthoinfo.aaos.org/topic.cfm?topic=A00139
Peripheral nerve surgery
San Francisco nerve pain sufferers—find relief from chronic nerve pain with peripheral nerve surgery. San Francisco peripheral nerve surgery treats nerve pain caused by nerve disorders and nerve injuries. Relief from chronic pain is possible through peripheral nerve surgery. Surgery that affects the nerves, usually caused by a nerve disorder or nerve injury, and causes chronic nerve pain.
What is it?
Peripheral Nerve Surgery can be performed throughout the body on any nerve that has been damaged or negatively affected by a related disorder. A systematic illness or infection can also cause the brain to nerve responders to misfire. The primary goal of surgery is pain relief. There are several procedures that fall under peripheral nerve surgery. Dr. Abbi runs diagnostic tests as well as completes a physical exam to determine which type of peripheral nerve pain surgery is right for each patient. In most cases this refers to where in the body the surgery will be performed and which nerves are affected.Purpose
The main purpose of peripheral nerve surgery is to relieve pain in the nerves, often caused by compression or injury. These nerves often regenerate themselves but in some cases that regeneration fails. When this happens, San Francisco nerve pain sufferers turn to peripheral nerve surgery to relieve chronic nerve pain caused by a nerve disorder, a nerve injury, a systemic illness or an infection. The surgery is successful because it structurally repairs the nerves in the body and fixes misfired that occur between the nerves and the brain.Benefits compared to other treatments:
Peripheral nerve surgery is more effective than other treatments because it targets the underlying cause and not just the symptoms. During surgery, Dr. Abbi performs a structural repair to offer significant pain relief. As an added bonus, some of the procedures can be done as minimally invasive surgeries, which means less recovery time and a shorter surgery in general. Not everyone, however, is a candidate for minimally invasive procedures.Areas the surgery helps:
San Francisco peripheral nerve surgery fixes misfires between the brain and nerves throughout the body that cause pain. The surgery can relieve nerve pain all over as well as increase motor function.What conditions can be treated?
San Francisco peripheral nerve surgery addresses nerve injury, pinched nerves, neuroma, motor dysfunction, tumors, nerve disorders, chronic pain and chronic pain conditionsThe procedure:
The length of surgery depends on what type of peripheral nerve surgery is being done. The steps of the procedure vary depending on what type of peripheral nerve surgery is being done. In most cases the goal is to relieve pressure on the nerve. In this case:- The patient is placed under general anesthesia.
- The surgeon uses small incisions to access the affected nerve(s).
- In some cases the surgeon will divide and reroute the nerves to eliminate pain. In most cases pressure is simply relieved from the nerves.
- The incisions are closed.
- The patient is closed and wheeled to recovery.

